In sixteen years of hanging out with feet I’ve seen my share of plantar fasciitis and other painful foot conditions. Let me walk you through the most common risk factors I see contributing to plantar fasciitis, ways to address them, what goes into determining a reflexology diagnosis*, and some suggestions for self-care I use in treatment plans.
Risk Factors
The foot and ankle come equipped with 28 bones, 34 joints, 112 ligaments, 3 arches, and have 34 muscles involved in movement and weight bearing (Webster, Murphy 2017). There’s a variety of things that can contribute to foot pain, in particular plantar fasciitis, and I’d like to outline some of the more common ones I see in my practice.
Footwear
Our ancient ancestors designed coverings for the feet to keep them warm, dry-ish, and prevent lacerations and abrasions, like this 5,500 year old moccasin. I’ve found many modern shoes restrict the natural motions of the feet as well as inhibit sensory input and thus motor output. Unshod gait activates joints and tissues from the feet all the way to the cervical spine, while rigid footwear decreases some of this activity (Franklin et al 2015, Wirth et al 2011).

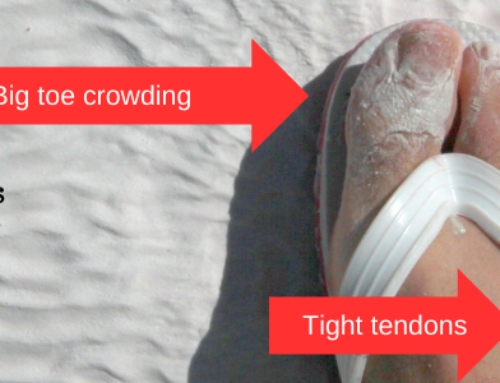
Seen here, I’ve illustrated some of the challenges we see with modern shoes.
I’ve created a quick illustration here of a typical maximalist shoe and I’d like to challenge you to take a peek in your closet and see if you can find a pair of shoes that don’t feature a toe spring and heel lift. As you can see from this image, modern shoes have a rigid toe spring and heel lift. Think about the arch as a bridge with supports in the forefoot and hindfoot, and the fascia as that horizontal flex that spans the two. When we lift the heel the fascia tugs on the metatarsophalangeal joints. When we lift the toes the fascia tugs on the calcaneus and thus the Achilles tendon. When we lift both we’re essentially asking the arch to move downward to accommodate the shortened fascia. Let’s take a closer peek at these challenges for the feet:
- Toe spring – the toes are lifted off the ground constantly with what’s known as a rigid toe spring which handicaps and weakens the foot’s muscles, leaving them vulnerable to plantar fasciitis (Sichting et al 2020);
- Heel lift – when the heel is lifted we see changes in the length of stride, body weight shift forward to the forefoot, pressure is decreased on the fascia at the calcaneus but is transferred instead to the ball of the foot at the metatarsophalangeal joints. This lift creates strain all the way up the posterior line of the body from the calves to the hamstrings, the sacral and lumber spine up to the neck. By raising the heel we lose ankle range of motion (ROM) for dorsiflexion, where the shin bone is drawn towards the toe when we walk. This has been found to lead to:
- Bunions;
- Hammertoes;
- Arch collapse;
- Plantar fasciitis;
- and Achilles tendinopathy (Richie 2018).
- Rigid shoes – prevent the natural rolling gait of the foot when walking and running, and hold the foot in an abnormal state of tension when standing;
- Narrow toe box – the narrow toe box of modern shoes create pressure on one of the other arches of the foot that spans the ball of the foot from the great toe to the little toe. When the shoe is too narrow for a normal foot this can kick start deformations like bunions, hammer toes, stress fractures in the metatarsals (these are the long foot bones in the middle of the foot), and Morton’s neuromas (Goud et al 2011). In a healthy foot the toes are the widest part of the foot – do your shoes reflect that?
The lovely Katy Bowman of Nutritious Movement shares tips on what to look for in foot-friendly shoes in her book Simple Steps for Foot Pain Relief:
- Heel should be flat to a maximum of 1/4″ lift;
- Toe box should be wide leaving the toes free to move around;
- Toe of the shoe should not be lifted but should sit flat on the floor – she recommends stacking heavy books on a pair of shoes that otherwise meet the foot-friendly guidelines to reduce or eliminate the toe spring and I’ve found this has worked for a couple of sandals;
- Sole should be thin and flexible to allow for proper foot biomechanics – you should be able to wring your shoe like a rag or sock and flex it back and forth.
When I’m not barefoot, my favorite footwear the past few years have included my Olu Kai sandals for warm weather, my Fitkicks for cooler weather or whenever I need a closed toe shoe, my trusty Skinners when I need something more rugged than the Fitkicks (yep, they’re basically a sock with a glass resistant material), and VivoBarefoot’s Jing Jing ballet flat when I need something more dressy. I still have a pair of Merrell’s barefoot glove shoe they partnered with Vibram soles for years ago that I break out every now and again. If I was going to add a shoe to a shopping cart right now I’d consider Xero’s leather flat, or Minnetonka’s softsole moccasin.
Hormones
Estrogen influences foot pain by reducing the rigidity of tendons and ligaments. We would anticipate high estrogen levels in a natural menstrual cycle following bleeding and just before ovulation, and in pubescent bodies with or without menstruation. Persons with hypothyroidism are susceptible to higher levels of estrogen due the relationship between the ovaries and thyroid falling out of balance. Are you due for a hormone lab panel soon?
Dry Constitution
A classic Vata dosha symptom is scanty lubrication of the sinews of the body. Those of us with a high amount of air, ether, or dryness in our constitution are missing that juiciness in the joints, tendons, and ligaments other constitutions have more of. I love seeing a Vata-pacifying diet, and demulcent herbs improve plantar fasciitis!
What about other constitutions and foot pain? A fire constitution (say Pitta) may experience excess heat which can translate to an increase in inflammation of the feet and would be addressed using a Pitta-pacifying diet, with cooling herbs. A water constitution (like Kapha) that is having excess dampness and stagnation will often report edema and swelling in the feet and would be addressed using a Kapha-pacifying diet, with warming and drying herbs.
Sedentary Lifestyle

Plantar Fascia on the Sole of the Foot, Image by Kosi Gramatikoff
Occupations that have us standing or sitting for eight hours a day put a strain on the musculoskeletal and cardiovascular systems.
Standing and sitting for long periods of time creates localized hypertension in the feet and lower legs as the calf muscles are not being activated to squeeze the blood vessels and return deoxygenated blood back to the heart. Poor oxygen supply to the feet through the tarsal tunnel can result in tissue necrosis like we see with plantar fasciosis. Dysfunction in the gastrocnemius and soleus muscles of the calf due to inactivity and/or wearing high heels can also lead to tarsal tunnel syndrome, a type of neuropathic pain similar to carpal tunnel syndrome we see in the wrists, but that shows up on the bottom of the foot.
Remember those 34 foot joints I mentioned earlier? Each of those are designed to articulate, absorb shock, and change the shape of the foot in motion. Our feet are designed for movement, and the less they move the more challenges we are likely to face. Tension and weakness within the musculoskeletal system are very likely to show up in one form or another in the feet.
In the vein of slow-and-steady turtles everywhere, I advise easing into a fitness routine like walking, jogging, and so forth. I recently read How to Get Your Feet in Walking Shape and love the tips they sourced from foot experts on how to prep your feet to go from sedentary to active without the foot pain in between.
Healing Plantar Fasciitis

Gray’s Plantar Aponeurosis, Anatomy of the Human Body, 1918
Now that we’ve got a better sense of what contributions there are to plantar fasciitis let’s look at what might go into a treatment plan.
Reflexology Diagnosis
*In reflexology we diagnose based on the reflex areas, not the corresponding areas of the body. It’s not my job to diagnose a client with whiplash of the cervical vertebrae 3-4. It is my job to detect congestion of the reflex areas of C3-C4, which makes that a reflexology diagnosis. Now, if you don’t tell me you were in a motor vehicle accident I will wonder why those reflex areas are so talkative but I won’t know if it’s caused by inflammation of the nerve fibers from a head-forward posture, a recent whiplash injury, or if there’s phrenic nerve involvement and I should connect the liver reflex congestion I feel later in the session, or chalk it up to poor footwear.
A peep into what I’m palpating and looking for in a reflexology session with someone experiencing foot pain:
- Toes – are the interphalangeal joints articulating well? Is there shortening in the extensor or flexor tendons resulting in the toes being drawn into flexion or extension when at rest?
- Forefoot – is there fluid movement in the plantar and dorsal interossei muscles? Are the metatarsal-phalangeal joints articulating on all axis points?
- Midfoot – how’s the intertarsal joints articulating? Are the metatarsal-tarsal joints restricted or have normal ROM? Is the master knot of Henry painful? How do the longitudinal and transverse arches feel and look?
- Ankle – how’s ROM for dorsiflexion, plantarflexion, eversion and inversion? How are the malleolar bursas?
- Hindfoot – is the Achilles attachment telling us anything? How about the retrocalcaneal, calcaneal, and subcalcaneal bursas?
Once I have an understanding of my client’s health history and I’ve gathered information from the feet I can make what we call a reflexology diagnosis, in which I’m drawing on an understanding of the anatomical structures of the foot and the homuncular map of the body mirrored on the feet. I may find that the sensitivity my client is experiencing on the medial abductor hallucis lines up with their history of low back pain that ties into energetic weakness in the kidneys and is showing up in the bladder reflex area over the medial talonavicular joint. Seeing as the tarsal tunnel runs right into this reflex area it would not be unusual to see a client with plantar fascia pain also reporting urinary system symptoms, for example.
Another example of a reflexology diagnosis with plantar fasciitis might be what I see when an elevated heel causes shortening in muscles of the legs and low back, which tilts the pelvis anteriorly, forcing the uterus to make concessions and tilt posteriorly, the change in uterine position creates painful cramps and tugs on the anterior pelvis, and the plantar fascia pain is along the reflex areas for the round ligaments and insertion at the pelvic floor reflexes right where the subcalcaneal bursa is really pissy.
Sometimes the foot is just the foot but when the whole body is this interconnected the reflexology diagnosis is rather interesting!
Foot & Lower Leg Workout
Unless the client is awaiting surgery to file down a bone spur growing directly into the aponeurosis band of tissue from the calcaneus, I give tips and suggestions on ways to stretch and exercise their feet to reduce pain and increase mobility and range of movement based on what I’m finding in the feet and their health history. Here’s some examples:
- Tight calves – place the ball of the right foot on a rolled up towel, using a wall for balance bring the left foot in front, creating a gentle stretch down the calf of the right foot. Repeat on the opposite side. Calf Stretch with a Towel Roll (video)
- Tight hamstrings – place the heel of the right foot on a chair, pivoting at the hips gently draw the upper body towards the right foot, protecting against rounding the lower back. Repeat on the opposite side. Static Hamstring Stretch (video)
- Tight toes – prepare a warm, not hot, sea salt or Epsom salt foot soak and add marbles or coin-sized pebbles. Soak feet for a few minutes then begin using the toes to grasp the marbles or pebbles, and remove one at a time from the soaking vessel, placing them on a adjacent towel on the floor. Marble pickup (video)
- A, B, C’s – while seated, point the toes of the right foot at the opposite wall and trace the alphabet in the air. Stop when the foot is fatigued and repeat on the other foot. Work at this until you can comfortably trace beyond the letter J. Alphabet exercise (video)
- Rub your feet – before bed, after walking, and upon rising, rub your feet using a favorite lotion, cream, or balm. Rotate the toes, twist and stretch the arch area, gently knuckle the heels. Self foot massage (video)
- Plantar Fascia stretch – while seated, bring your left ankle up to your knee to sit in a figure four position. Let the knee drape naturally, being mindful not to push or force it, especially with hip flexor tension. Reach the left hand forward to the toes and gently stretch the toes towards the knee, creating a nice stretch across the bottom of the foot. Hold the stretch for 15-20 seconds and repeat on the opposite leg. Plantar Fascia stretch (video)
Resources
I’ve included links to books on GoodReads to check out reviews and see if they’d be a good fit for your library. I’ve also included a couple of videos for basic range of motion assessments. If you’re not in the Austin, Texas area but want to work with a reflexologist I recommend visiting the American Reflexology Certification Board’s online directory of board certified reflexologists like myself. The Reflexology Association of America has an online directory of their qualified members.
- Simple Steps to Foot Pain Relief: The New Science of Healthy Feet by Katy Bowman, 2016
- Barefoot Walking: Free Your Feet to Minimize Impact, Maximize Efficiency, and Discover the Pleasure of Getting in Touch with the Earth by Michael Sandler and Jessica Lee, 2013
- Fix Your Feet: Build the Best Foundation for Healthy, Pain-Free Knees, Hips, and Spine, by Philip Maffetone, 2004
- The Good Foot Book: A Guide for Men, Women, Children, Athletes, Seniors–Everyone by Glenn Copeland, with Stan Solomon
- Walking Meditation: Easy Steps to Mindfulness by Nguyen Anh-Huong and Thich Nhat Hanh
- The Walking Deck: 50 Ways to Walk Yourself Healthy by Shirley Archer, illustrations by Ann Field
- Passive Range of Motion Assessment (video)
- Active Range of Motion Assessment (video)
References:
- Chaitow, L., & DeLany, J. (2011). Clinical application of neuromuscular techniques, Volume 2 E-Book: The leg and foot. Elsevier Health Sciences. 503-577.
- Franklin, S., Grey, M. J., Heneghan, N., Bowen, L., & Li, F. X. (2015). Barefoot vs common footwear: a systematic review of the kinematic, kinetic and muscle activity differences during walking. Gait & posture, 42(3), 230-239.
- Goud, A., Khurana, B., Chiodo, C., & Weissman, B. N. (2011). Women’s musculoskeletal foot conditions exacerbated by shoe wear: an imaging perspective. Am J Orthop (Belle Mead NJ), 40(4), 183-191.
- Richie, Douglas. (2018). Heel Elevation In The Shoe: What The Literature Reveals. Podiatry Today, 31 (11), 30-41.
- Sichting, F., Holowka, N. B., Hansen, O. B., & Lieberman, D. E. (2020). Effect of the upward curvature of toe springs on walking biomechanics in humans. Scientific Reports, 10(1), 1-11.
- Webster, J., & Murphy, D. (2017). Atlas of Orthoses and Assistive Devices E-Book: Chapter 19 Foot Biomechanics. Elsevier Health Sciences. 216-228.e1.
- Wirth, B., Hauser, F., & Mueller, R. (2011). Back and neck muscle activity in healthy adults during barefoot walking and walking in conventional and flexible shoes. Footwear Science, 3(3), 159-167.







[…] gripping to keep them from falling off are one of the leading causes of foot pain, including Plantar Fasciitis, that I see in my Austin […]